Silent
Silent provides the tools for seekers to recognize their path and enables self-reliance for spiritual and magickal growth.
Seekers gain insight from his work and find their inner calm from his ability to listen and help others reflect.
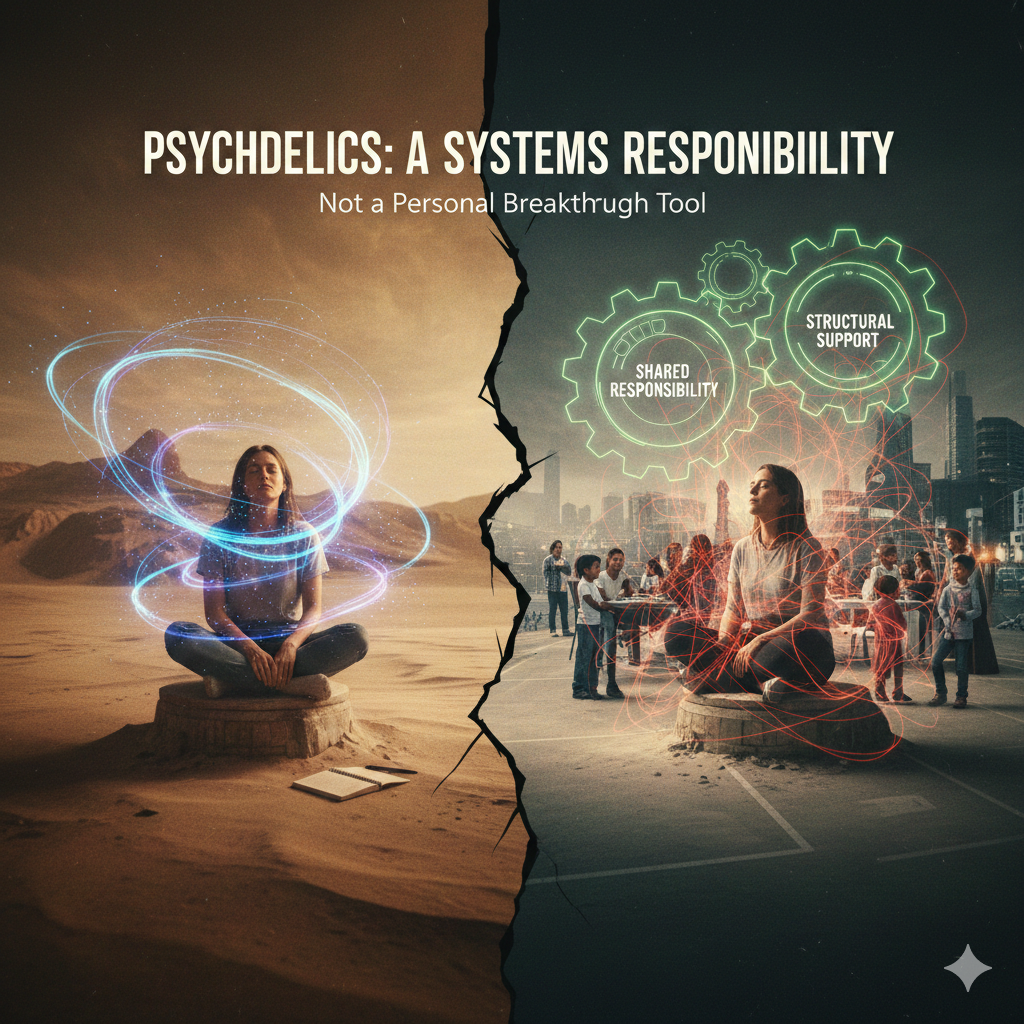
There is a quiet but consequential mistake embedded in much of today’s psychedelic discourse: the belief that transformation is primarily an individual achievement.
A journey is framed as personal insight. Healing is treated as a private awakening. Integration is often reduced to self-reflection and journaling.
This framing is not just incomplete. It is unsafe.
For clinicians, practitioners, and regulators, psychedelics must be understood not as isolated peak experiences but as systemic interventions. These substances do not act on individuals in a vacuum. They interact with families, workplaces, cultures, legal structures, and care systems. When we fail to account for those systems, we shift risk downward and responsibility away from the very institutions that enable these experiences.
The Fallacy of the Isolated Journey
The “isolated journey” narrative is appealing because it is simple. One person. One session. One breakthrough.
But this framing ignores a fundamental truth: psychedelics reliably dissolve boundaries, not only within the psyche but between the individual and their environment. Values shift. Identity loosens. Relationships are reinterpreted. Authority structures are questioned. Meaning is re-authored.
When systems remain unchanged but the individual is altered, friction is inevitable.
A clinician may see a powerful insight and call the session a success. A facilitator may celebrate emotional catharsis. Yet the real test begins afterward, when the individual returns to the systems that shaped them in the first place. Insight without structural support is not healing; it is exposure.
Family, Work, and Cultural Re-Entry Failures
Most harm does not occur during psychedelic sessions. It occurs during re-entry.
A person returns home with new boundaries, but their family system is unchanged.
They return to work with a reoriented sense of purpose, but the organization still rewards compliance over coherence.
They return to a culture that has no language for non-ordinary states, no rituals for integration, and no tolerance for ambiguity.
We call this “integration work,” but too often we treat it as an individual responsibility. Meditate more. Journal longer. Find a coach. Regulate yourself back into systems that have not earned your regulation.
This is a category error. Re-entry is not a personal failure. It is a systems failure.
If psychedelics reliably increase sensitivity, authenticity, and boundary awareness, then unsupported re-entry can destabilize marriages, careers, and identities. When this happens, the individual is often pathologized for “not integrating well,” when in reality they are encountering the limits of their environment.
Organizational Responsibility for Downstream Effects
Psychedelics do not end when the session ends. Neither does responsibility.
Clinics, training programs, retreat centers, and regulatory bodies all participate in shaping downstream outcomes. When they design care models that stop at the moment of insight, they externalize risk onto the participant’s life.
A systems-responsible model asks harder questions:
What happens when someone’s values change faster than their economic reality?
What support exists when insight disrupts relational contracts?
What governance structures are in place when meaning-making accelerates but social context does not?
Healthcare systems would never approve a surgical intervention without post-operative care, yet psychedelic care models routinely do the equivalent. The result is predictable: avoidable harm, silent suffering, and a growing gap between promise and practice.
Why “Personal Insight” Is Not a Care Model
Insight is not treatment. Insight is not integration. Insight is not stability.
Insight is raw material.
Without relational scaffolding, cultural containers, and longitudinal support, insight can become disorganizing rather than liberating. It can isolate individuals from their communities. It can erode trust in institutions without offering viable alternatives. It can leave people awake but alone.
For regulators, this is not a philosophical concern; it is a governance issue. Any intervention that predictably alters worldview, identity, and relational dynamics must be evaluated at the systems level. Risk assessment must include social destabilization, not just acute physiological safety.
For clinicians and practitioners, this requires a shift in professional identity. The role is not to facilitate awakening and step away. It is to steward transitions across time, context, and relationship.
A Systems-Oriented Call to Action
If your model ends when the session ends, it is incomplete by design.
This is not about slowing progress. It is about maturing it.
Psychedelics reveal what systems conceal. That makes them powerful. It also makes them dangerous when treated casually. The future of this field depends not on deeper journeys, but on deeper responsibility.
Transformation does not happen in isolation. Neither should care.
ABOUT THE AUTHOR

Silent
Silent provides the tools for seekers to recognize their path and enables self-reliance for spiritual and magickal growth.
Seekers gain insight from his work and find their inner calm from his ability to listen and help others reflect.